USEMS-FSEM 2025 Essay Competition Winner Announcement
The Faculty of Sport and Exercise Medicine UK (FSEM), in collaboration with the Undergraduate Sport and Exercise Medicine Society (USEMS), have announced Mr Nicolas Chapelot as the winner of the 2025 Essay Competition.
Mr Chapelot is a medical student at University College London, originally from Cambridge, with a long-standing interest in sport and exercise. He competed in track sprinting at school and later played rugby at university. His interest in Sport and Exercise Medicine developed further following two ACL and meniscal injuries requiring reconstruction, which highlighted the importance of rehabilitation, injury prevention, and long-term musculoskeletal health.
He is particularly interested in preventive medicine and the role of exercise and nutrition in metabolic health. He chose this topic due to widespread misinformation around weight, diet, and newer obesity treatments. Weight alone is a limited measure and often distracts from more meaningful outcomes such as body composition, physical function, and long-term health. He believes obesity management should prioritise sustainable, evidence-based approaches rather than weight loss in isolation.
His essay, “Rethinking Obesity Treatment: Why Resistance Exercise Prescription Must Move to the Forefront”, was praised for its clear structure, compelling argument, and confident stance. The editorial presents a strong justification for the topic and articulates a well-defined opinion, effectively challenging conventional approaches to obesity management. Mr Chapelot highlights the risks of weight loss strategies that neglect exercise, and makes a persuasive case for resistance training as a central, evidence-based intervention.
If you would like to learn more about the next iteration of the competition, you can view information via the link below.
Congratulations to Nicolas for this excellent piece of work. Mr Chapelot’s winning essay is presented below.
Rethinking Obesity Treatment: Why Resistance Exercise Prescription Must Move to the Forefront
In the UK, the average lifespan is around 81 years, but the health span is significantly shorter at just 63 years, resulting in many adults spending nearly two decades in poor health. Obesity plays a major role in this decline, contributing to metabolic syndrome, cardiovascular disease, and cancer. With the UK having one of the highest obesity rates in Europe, 29% in 2022 1, projected to reach 36% by 2040 2, the strain of this epidemic on the already struggling healthcare system is undeniable. To address this, the focus must shift beyond obesity alone to key health markers. While diet remains the most effective tool for weight loss, exercise prescription, particularly resistance training, is essential for these health markers, enhancing insulin sensitivity, and preserving muscle mass during weight loss. I argue that in light of this, resistance training must be “pushed to the forefront” and integrated alongside diet in obesity management.
A Holistic Approach to Obesity Management
Is an obese person necessarily unhealthy? I’d argue not, considering how a professional rugby player may be classified as obese due to their high muscle mass despite being in peak physical health. This is a clear example of how despite being an excellent metric on an epidemiological basis, BMI has failed to account for body composition and key metabolic biomarkers essential for characterising health. Hence, the focus needs to shift away from arbitrary weight classifications and toward a more holistic approach, rather than relying solely on BMI3. This can be done by incorporating body composition metrics via DEXA scans and blood biomarkers. In research regarding dietary intervention and exercise prescription, this change has improved strategies in obesity management, enhancing metabolic health, weight loss, and overall well-being 3.
The Importance of Muscle Mass for Longevity
Muscle mass is crucial for healthy ageing, particularly during the “marginal decade” (ages 60–70), where strength and function significantly decline. Hence, maintaining and building muscle strength and mass is essential to protect against sarcopenia and its consequences of frailty, falls, and dependency. This is highlighted in research showing the link between low levels of muscle mass and a higher risk of mortality (see Figure 1) 4.
Additionally, low muscle mass is an independent risk factor for all-cause mortality and cardiovascular disease. This effect on mortality was even greater for those with poor metabolic health or obesity, perhaps due to muscle tissue acting as a metabolic reservoir for glucose regulation and insulin sensitivity 4. This highlights the greater importance of maintaining and increasing muscle strength in those groups.
Figure 1: The Importance of Muscle Mass for Longevity
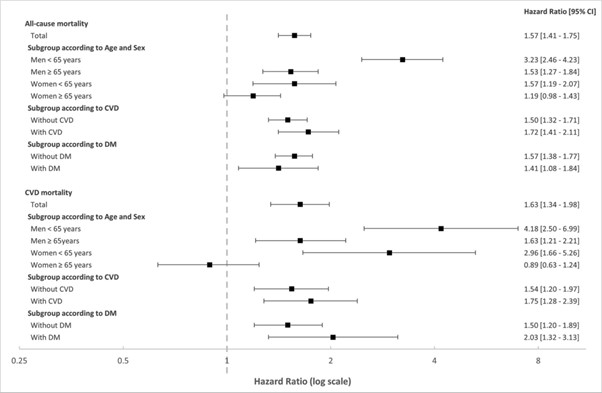
Figure 1: The Hazard ratios for all-cause and cardiovascular disease (CVD) mortality based on low muscle mass. Adjustments were made for age, sex, race, smoking status, alcohol consumption, estimated glomerular filtration rate, body composition, history of cancer, hypertension, diabetes mellitus, dyslipidaemia, and prior cardiovascular disease events 4.
Risks of Weight Loss Without Exercise
How is weight loss achieved? Weight loss is fundamentally driven by maintaining a caloric deficit—an undeniable principle rooted in the first law of thermodynamics. However, the intricacies of the “calories in, calories out” equation go far beyond simple math and are a strongly debated topic. Ideally, weight loss would come primarily from adipose tissue. However, in a hypocaloric state, the body is efficient at breaking down understimulated muscle tissue—especially when combined with a sedentary lifestyle and inadequate protein intake. Unfortunately, this scenario is common, resulting in worsened body composition and, worst case, sarcopenic obesity. This issue has been highlighted by the popularity of pharmacological interventions like GLP-1 receptor agonists (e.g., Semaglutide), which create large caloric deficits, often composed of low-nutrient-dense foods and lack of resistance training 5.
Thankfully, maintaining lean mass during weight loss is possible with the right approach. By ensuring adequate high-quality protein intake and incorporating resistance training into weight loss interventions, muscle tissue can be preserved 6. Furthermore, resistance training not only helps preserve muscle mass but also enhances dietary interventions by improving body composition and markers of metabolic health such as cholesterol levels and insulin sensitivity (see Figure 2) 7. Additionally, high-intensity or interval endurance training proves more effective than moderate-intensity, steady-state cardio for metabolic benefits 8. This suggests that combining resistance training with high-intensity exercise and an energy deficit may be the most effective strategy for improving overall health in obese populations.
Figure 2: Change in Cardiometabolic Risk Factors After 6 Months of CR and Exercise Treatment
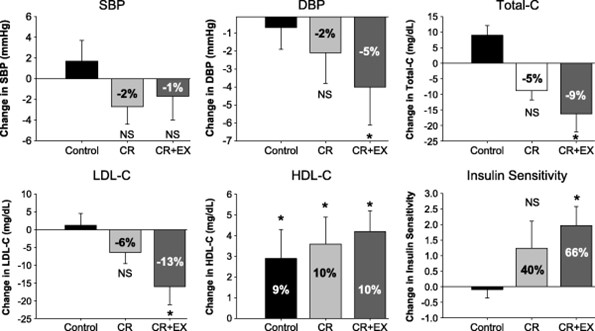
Figure 1: The Hazard ratios for all-cause and cardiovascular disease (CVD) mortality based on low muscle mass. Adjustments were made for age, sex, race, smoking status, alcohol consumption, estimated glomerular filtration rate, body composition, history of cancer, hypertension, diabetes mellitus, dyslipidaemia, and prior cardiovascular disease events 4.
Conclusion
Diet remains the leading strategy for initial weight loss. Alone, it falls short in preserving muscle mass, improving body composition, and addressing long-term health outcomes. However, when combined with exercise, particularly resistance training, the benefits on health are enhanced and pitfalls reduced. The fight against obesity should not prioritize short-term weight loss at the expense of long-term health. We must redefine success in obesity management to include metrics beyond BMI, focusing on quality of life, metabolic health, and longevity. By looking at this issue through this lens, exercise prescription, especially resistance training, is not merely “one of the pack” in obesity management; it is the linchpin for sustainable health and well-being. It’s time to move beyond solely focusing on diet, with resistance training as a cornerstone of obesity treatment and public health weight management programs.
Runner Up – Exercise Prescriptions in Obesity: Why Plans Are Just as Important as Pills
The panel also extended special recognition to this year’s runner-up, Dr Marian Bhaskar. Dr Bhaskar graduated in 2023 and (at the time of submission) was serving as an FY2 doctor with the South Eastern Health and Social Care Trust under NIMDTA in Northern Ireland.
Her essay, “Exercise Prescriptions in Obesity: Why Plans Are Just as Important as Pills”, was praised for its clarity, structure, and thoughtful engagement with the topic. The editorial presents a well-balanced argument, effectively positioning exercise as a vital component in obesity management while acknowledging the role of other interventions. Her use of evidence and references was particularly strong, and her reasoning was consistently logical and well-supported. The essay concludes with a clear recommendation for action, encouraging a shift in how we measure and value the benefits of exercise in clinical settings.
Dr Bhaskar’s work was commended for its insightful contributions to the discussion and its relevance to evolving perspectives on obesity as a complex, multifactorial condition.
Conclusion
The USEMS-FSEM Essay Competition continues to highlight the passion, intellect, and creativity of emerging professionals in Sport and Exercise Medicine. It serves not only as a showcase for academic excellence, but also as a platform for future clinicians to engage with real-world challenges and propose innovative, evidence-based solutions. Through thoughtful analysis, clear communication, and a commitment to improving patient care, entrants continue to demonstrate the importance of Sport and Exercise Medicine in shaping modern healthcare.
Bibliography
- National Health Service (NHS) Digital. Health Survey for England, 2022 Part 2: Adult Overweight and Obesity. 24 Sep 2024. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2022-part-2/adult-overweight-and-obesity
- Cancer Research UK. A new analysis estimates over 21 million UK adults will be obese by 2040. 19 May 2022. Available from: https://news.cancerresearchuk.org/2022/05/19/new-analysis-estimates-over-21-million-uk-adults-will-be-obese-by-2040/?utm_source=chatgpt.com
- Gallagher D, Deurenberg P, Heymsfield SB, et al. Chapter 5: Body composition and physical activity. In: Stewart T, editor. Physical Activity and Health: An Interactive Approach. 2024. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6690141/
- McGlory C, Phillips SM. Muscle mass loss during weight loss: effects on metabolic rate and glucose metabolism. J Cachexia Sarcopenia Muscle. 2023;14(1):21-31. doi: 10.1002/jcsm.13397. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/jcsm.13397
- Sztalryd C, O’Brien E, Britton C, et al. Impact of GLP-1 receptor agonist use on lean mass in obesity treatment: a randomized controlled trial. Diabetes Obes Metab. 2024;26(2):396-405. doi: 10.1111/dom.15271. Available from: https://pubmed.ncbi.nlm.nih.gov/38937282/
- Nowicki A, Gąsior Z, Wojciechowski J, et al. Obesity and its metabolic consequences: an updated review. Qual Soc Sci. 2024;29(2):118-126. Available from: https://apcz.umk.pl/QS/article/view/57000
- Ross R, Janssen I, Dawson J, et al. Caloric restriction with or without exercise: the effect on body composition and fat distribution. Med Sci Sports Exerc. 2010;42(1):92-98. doi: 10.1249/MSS.0b013e3181b0c5d1. Available from: https://journals.lww.com/acsm-msse/fulltext/2010/01000/caloric_restriction_with_or_without_exercise__the.20.aspx
- Papamichael N, Ellis C, Symonds ME. The effect of exercise on body composition and muscle mass in obesity: A systematic review. Diabetol Metab Syndr. 2015;7:45. Doi: 10.1186/s40200-015-0154-1. Available from: https://link.springer.com/article/10.1186/s40200-015-0154-1